Clinical staffing shortages, particularly nursing, pre-date COVID-19 by decades, but the pandemic and its effects on the profession and economy have taken an even greater toll. A November report from the U.S. Bureau of Labor Statistics showed that 450,000 workers have left the healthcare industry since February 2020, with the vast majority coming from nursing or residential care facilities.
As a result, the competition for nurses among hospitals has become fierce. Some hospitals and health systems have been forced to limit capacity due to staffing shortages. Faced with these challenges, hospitals need to ensure safe and effective care while at the same time maximizing efficiency for nurses and other clinicians who may be practicing with smaller teams.
Emergency medical interventions ideally demonstrate how hospitals can solve both dilemmas. Such life-saving interventions can occur daily or even more often depending on hospital size and specialty. By delivering live, streaming, surveillance-level data throughout the hospital, not just in critical care units, medical emergency teams (METs) or rapid response teams (RRTs) can be better prepared to deliver care, but also better able to prevent emergencies in the first place.
Surveillance Data vs. Early Warning Score
Sometimes a medical emergency offers no warning, but in most instances, signs of decompensation appear in the patient that can inform a clinician that a life-threatening event may occur, particularly in decompensation related to respiratory depression leading to respiratory failure and arrest. [1] [2] Signs of early deterioration leading to ICU transfers and cardiac arrest have been documented, and the signs of respiratory distress and insufficiency have been recognized as a key finding in identification of patient deterioration on the general care floor (GCF), with “every hour of delay in detecting patient deterioration on the GCF” translating into an increased risk of death in the ICU by 1.5%. [3]
To support clinicians in detecting these events, early warning scores are available. These tools, while useful and aid in clinical decision-making, offer only a limited perspective on a potential adverse event. Early warning scores are much like a weather report indicating that your community will receive two feet of snow by tomorrow. While certainly helpful, the warning lacks key information, such as how fast the snow will fall and when. Will there be breaks in the storm? What precise areas will be most affected? Such information can help you form a plan, but also avoid wasting time and effort by shoveling too often, too early, or too late.
Conversely, surveillance data provides a continuous view of the patient that helps clinicians to detect decompensation trends before a resource-intensive, all-hands-on-deck response is required. In the snowstorm analogy, live-streaming data across multiple meteorologic data points could indicate when you should shovel and when the next wave of flurries will come through so you can conserve your energy and limit musculoskeletal exertion. Similarly, this holistic perspective of multiple vital signs over time may help identify trends that could enable clinicians to detect decompensation and the need for intervention. Earlier prevention of an adverse event also allows hospitals to better allocate staffing, drug, and equipment resources to help stabilize the patient.
RELATED READING: Smart Alert: A Harbinger of Adverse Events in Critical Care Settings
Every Minute Counts
When considering the importance of surveillance-level data in non-critical care settings, I am reminded of an elderly patient I was monitoring in ICU many years ago. The woman was being weaned from post-operative mechanical ventilation after coronary bypass surgery. It turned out the protocol ordered was too aggressive. Her heart rate rose from below 100 beats per minute to more than 100 and she began hyperventilating. In 25 to 30 minutes, the ventricular tachycardia alarm sounded on her bedside monitor and the hospital’s MET was activated. Fortunately, we were able to stabilize the patient and she suffered no injury.
This case example, however, reinforced for me how surveillance-level data of this patient could have avoided the code blue response. Knowing what we knew about that patient’s age, history, and condition, with her vitals steadily veering off course, we might have recognized the decompensation and stabilized her sooner. With preventive action, earlier is always better.
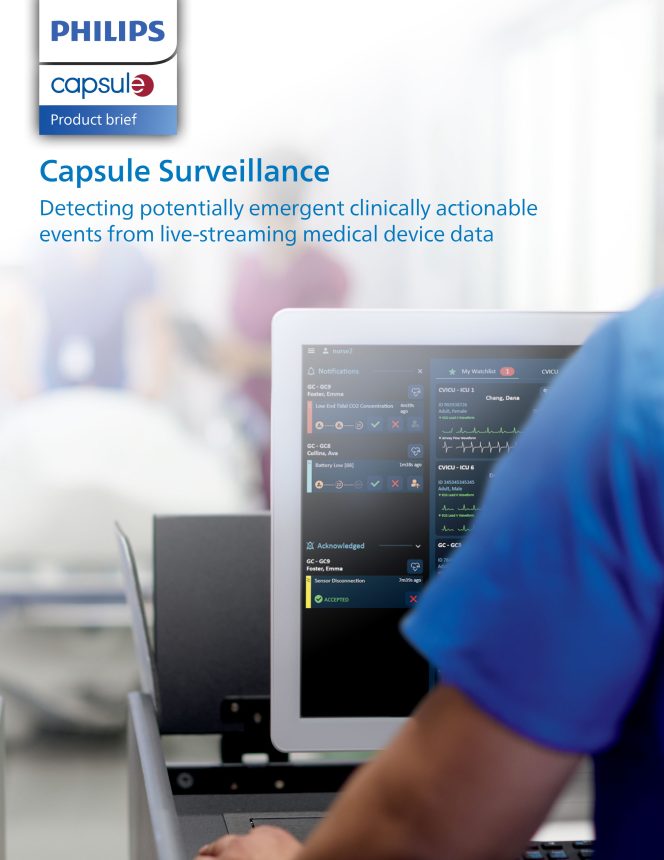
Inside the intensive care unit, surveillance-level insight is standard protocol, but in medical-surgical and other general care units, this is not always the case. Philips Capsule’s Clinical Surveillance Solution continuously analyzes comprehensive medical device data to help identify deterioration and assists in reducing the risk of life-threatening events. Live-streaming data delivered by Clinical Surveillance serves as a friendly tap on the shoulder to facilitate proactive care by sending notifications to the caregiver, regardless of location.
This early guidance could help protect the patient’s health and safety while enabling clinical staff to practice more efficiently during these challenging times.
About the author
John Zaleski, Ph.D., NREMT, CAP, CPHIMS is head of clinical informatics at Philips Capsule.
Learn more about Philips Capsule Surveillance.
Download