Emergency medical personnel, whether in the field or in the emergency department, are frequently faced with respiratory distress and failure and cardiac arrest. A key tool in monitoring and assessing cardiac and respiratory function, particularly when working with advanced airway placement, determining adequacy of chest compressions, and return of spontaneous circulation, is capnography, which provides immediate assessment of ventilation adequacy.
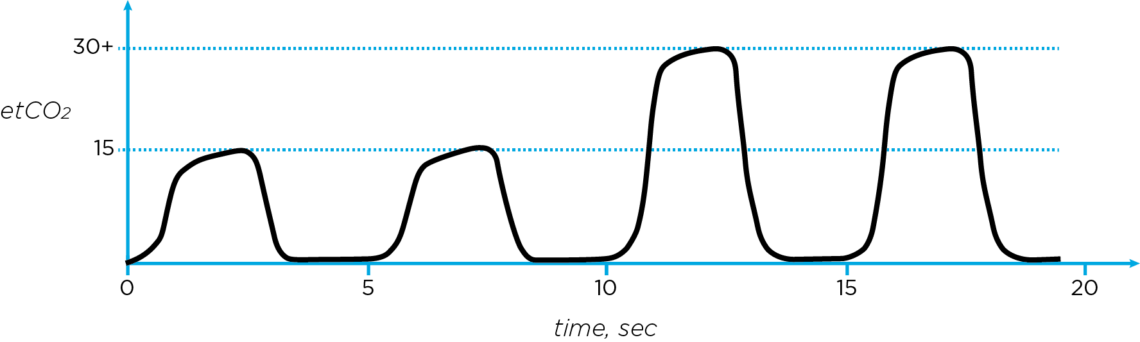
The key measure obtained from capnography, End-tidal carbon dioxide, or, is an indicator of active ventilation. In patients who are in cardiac arrest or who have an advanced airway (e.g.: supraglottic airways such as laryngeal mask airways and endotracheal tube intubation), the placement of the airway and its ability to transport air is directly discernible using end-tidal capnography. In patients who are in cardiac arrest, and for whom an advanced airway is in place, artificial positive-pressure ventilations are typically applied at the rate of eight-to-ten breaths per minute, or one breath every six-to-eight seconds. This contrasts slightly with non-intubated positive-pressure assisted ventilations, such as those using a bag-valve mask (BVM), in which, depending on the patient (i.e., adult versus pediatric versus neonate) will be one breath every three-to-five seconds, or roughly twelve-to-twenty breaths per minute [1] [2, pp. 506-526]. In the case of return of spontaneous circulation, end-tidal capnography may indicate values under fifteen mmHg, although experience has shown that this can vary widely. Capnography is also quite useful in guiding compressions in the case of cardiopulmonary resuscitation: in terms of providing feedback on effectiveness and rate of compression, which should be between one hundred and one hundred twenty compressions per minute. When a patient regains spontaneous circulation, a large increase to normal or elevated levels of end-tidal capnography are often seen as circulation begins to rid the body of excess carbon dioxide during exhalation and there is a return to normocapnia. This is illustrated in the plot of Figure 1 [3] [4] [5].
REALTED READING: Why Capnography is Essential for Postoperative Care
Capnography waveform typical of return of spontaneous circulation (ROSC) after cardiac arrest
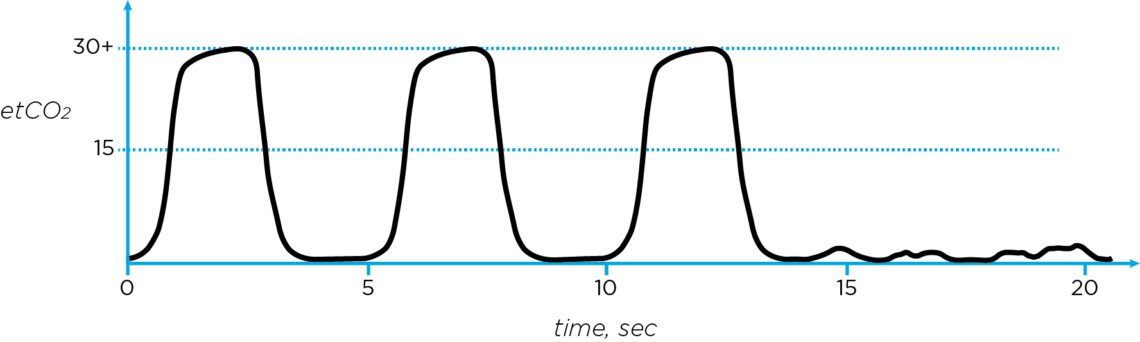
The displacement of an advanced airway can result in little to no air entering or exiting the lungs, and in this case the capnography waveform is lost, as is shown in Figure 2 [3] [4] [5]. It must also be noted that such an event may also be coincident with cardiac arrest, such as might be seen in a patient who is already intubated but lapses into asystole. Hence, capnography will indicate either the lack on effective ventilation that is due to displacement of the advanced airway, or the onset of cardiac arrest – both emergent events requiring immediate intervention.
Capnography waveform typical of displacement of an advanced airway
In summary, real-time feedback is obtained on ventilation and placement of advanced airways, adequacy of chest compressions, and the possible dislodgement of the airway. These findings are critical to ensuring maintenance of life functions. Capnography is an essential link in establishing the adequacy of airway patency, breathing, and circulation – the ABCs of vital assessments that are key to life. Vital signs and medical device data capture has always been the essential foundation of Capsule’s offerings, and with capnography, Capsule further underscores its commitment to patient safety.
John Zaleski, Ph.D., NREMT, CAP, CPHIMS is head of clinical informatics at Capsule Technologies.