It’s no secret that healthcare providers face ongoing pressures from staff shortages, complex patient conditions and systemic inefficiencies.
In fact, by 2030, the World Health Organization projects a shortfall of 11 million healthcare workers, creating gaps in access to care for millions of people.1 At the same time, data inefficiencies plague providers, with 77% of healthcare professionals reporting that they have lost clinical time due to incomplete or inaccessible patient data, according to the Philips Future Health Index (FHI) 2025 Global Report.2
The growing divide between demand for care and provider availability leads to longer wait times for care – globally 33% of patients report worsening health due to not seeing a doctor sooner – while the struggle for data availability creates frustrations for clinicians who lose valuable time – sometimes more than four working weeks per year – that could be better spent on patient care.2
All of this leads to greater challenges for patients and healthcare providers.
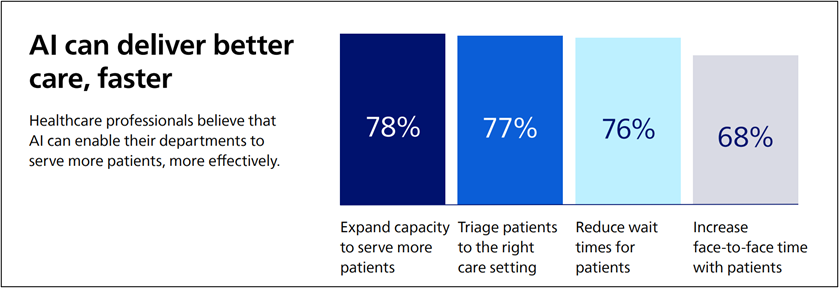
In the midst of these challenges, artificial intelligence (AI) holds promise for alleviating administrative burdens, streamlining workflows and helping to expand capacity so that clinicians have more time and patients get the care they need faster.
But just as importantly, AI holds the promise of unlocking the power of data for predictive medicine with a goal of helping to diagnose diseases more precisely to improve outcomes. In fact, 82% of healthcare professionals say AI and predictive analytics could save lives by enabling early interventions.2
Source: Philips Future Health Index 2025 Global Webpage
Further, according to a study by the National Bureau of Economic Research, wider adoption of AI could lead to savings of $200 billion to $360 billion annually in the U.S. alone.3
With so much potential benefit, how can health systems prepare and take advantage of what AI can offer?
To take advantage of the benefits promised by AI, healthcare providers need a technology foundation that will enable them to use all of their patient data in agile, innovative, new ways to augment clinical capacity. Health systems will need high-fidelity, contextualized, connected data that can power AI-enabled systems, alarm management, remote monitoring, clinical surveillance, clinical decision-support and other use cases that go far beyond static documentation in an electronic health record (EHR).
Last fall we talked about how to select a core medical device integration program. Now, we want to show how an advanced integration program can allow health systems to leverage their medical data further and set the foundation for an AI transformation that can help address the challenges of increasing workloads, burnout and complex patient conditions.
Industry-standard medical device integration typically refers to sending patient data from bedside devices, such as monitors, ventilators, balloon pumps, to the electronic health record. While documentation in the EHR is critical, the focus for most clinicians in the EHR is on continuous data received in intervals of one minute, a small subset of the data that’s available, and data from only a handful of medical devices.
By contrast, a smart alarm management system needs real-time, contextualized data that includes patient vitals associated with the alarms so that clinicians can see a complete picture of the patient’s condition.
Advanced integration fits the needs of those smart alarms and potential AI-powered predictive capabilities by sending high-fidelity patient data simultaneously to multiple third-party destinations for documentation, reporting, precision analysis and critical decision support. And, advanced integration allows for all the patient data to be transmitted — including vitals, alarms, and waveforms – in near real-time, in the correct frequency and format that the receiving system needs.
This means that with advanced Integration, real-time, contextualized data can be sent simultaneously to downstream systems for:
In this way, advanced integration lets health providers choose where patient data goes, and at what intervals, to best support their clinical needs.
Two prominent use cases that depend on advanced integration are remote monitoring and smart alarm management, both of which require real-time, contextualized data.
Remote monitoring might mean that a clinician managing patients can see all the data (vitals, alarms, waveforms), and apply analytics to identify patterns and trends that can help anticipate patient deterioration or an emergent event.
Smart alarm management might mean that a clinician rounding the floor with a handheld device such as Epic Rover receives an alert that shows the alarm, the patients vitals and other data to help enable appropriate, timely intervention.
Clinicians looking to take full advantage of advanced integration should look for these key benefits and characteristics:
Advanced integration can power additional use cases that include central station monitoring and virtual care (eICU), where integrated devices could provide a more complete view of the patient and support condition-specific oversight; quality improvement and research to identify patterns and trends; and clinical decision support tools to leverage real-time data from medical devices to enhance decision-making.
AI has the potential to relieve many of the burdens facing today’s healthcare professionals as well as to help expand care capacity and support predictive medicine. But to take advantage of all AI can offer, health systems need better access to complete patient data, and the ability to send that data to multiple systems, including AI-enabled systems, to transform raw data into contextualized, actionable information and insights.
Advanced integration makes data available to different clinical applications and can support a variety of use cases, beyond EHR documentation, to support real-time decision making with a goal of helping improve outcomes. As the challenges facing healthcare continue, the importance of leveraging data effectively across multiple systems, and in more contexts, to support a wider range of clinical use cases, including AI-enabled applications, will only grow.
Please let us know your thoughts about AI in your organization, and how we can support you in meeting your patient care needs with advanced integration features available through the Philips Capsule Medical Device Information Platform. Contact us today to speak with an expert about how implementing clinical data technologies might benefit your patients, or feel free to reach out to us directly at MDIProdMgmt@philips.com.
Christopher Cage is a Senior Product Manager working on Medical Device Integration and Data Management at Philips Capsule.
Learn more about device connectivity and Philips Medical Device Integration.
Download