Florence Nightingale, an English social reformer, statistician and the founder of modern nursing, wrote in 1859: “Unnecessary noise is the most cruel absence of care which can be inflicted either on sick or well.” [1]
Imagine what Nightingale would say if she were alive today!
Modern hospitals are awash in sound. Monitors, alarms, pumps and other equipment provide vital data to support clinical care, but also produce noise levels unheard of decades, let alone a century, ago.
One patient monitor in a typical, modern Intensive Care Unit (ICU) can produce between 200-400 alarms per patient, per day. Furthermore, most of these alarms are false or clinically insignificant, with 85–99% of all alarms being non-actionable. [2] Most hospital rooms house two patients separated by a curtain, which means each patient experiences a double whammy of beeps, buzzes and alarms.
Noise effects
All this noise negatively impacts patients, their families and the clinical staff.
- For patients, sleeping is healing. Sleep disruption from frequent and high levels of noise can produce confusion, anxiety and depression, and impairs the healing and recovery process. This contributes to a diminished patient experience and poorer outcomes.
- For the patient’s family, when an alarm sounds and time passes with no one attending to their loved one’s alarm, fear sets in. In most cases, either the patient, if capable, or the family member, presses the nurse call button or runs into the hallway searching for help. These instances can erode trust in the medical devices and the clinical staff, and lead to diminished patient satisfaction.
- For the clinical staff, reacting to alarms can constitute 35% of the working time of a nurse in a full ICU. [3] This sensory and cognitive overload caused by an excessive number of alarms can result in delayed reactions to alarms, or to staff prioritizing alarms based on patterns of “false alarms” or other available patient data, which may impact patient safety and lead to errors. This, along with moral distress, results in symptoms of sadness, frustration and anxiety which, in the long term, can lead to clinical staff burnout and job dissatisfaction. [4-6]
Why so much noise?
There are many root causes for the proliferation of non-actionable and clinically insignificant alarms. [7]
Among the most common is poor skin preparation for electrocardiograms (EKGs), improper electrode placement and pulse oximetry finger probes that become dislodged and cause alarm “misfires.”
Also common is inadequate battery management, resulting in “low battery” alarms, as well as devices unable to send data to central stations.
Alarm system settings can contribute to the problem – lack of standardization for default settings, inconsistent use of system features and default system limits that are too tight or not personalized can trigger alarms that are not clinically actionable.
Training and policies play an important role when it comes to alarm system settings, with inadequate training in alarm management policies and protocols, or lack of best practices for customizing alarm systems to actionable limits for each patient leading to random or inconsistent alarms.
Industry’s response
The perils of alarm mismanagement have caught industry and regulators’ attention.
- Joint Commission (JCAHO) has identified alarm management as a 2023 National Patient Safety Goal and requires hospitals to take action to reduce unnecessary alarms as a condition of accreditation.
- AACN (American Association of Critical Care Nurses) offers Updated Practice Standards outlining evidence-based protocols and clinical strategies that healthcare organizations can implement to address issues related to alarm management.
- AAMI Foundation National Coalition for Alarm Management Safety outlines improving the alarm management process through evaluating alarm settings, limits, delays, creating processes to customize alarm settings, and providing training to empower improvement, not only with the clinical staff but also with patients and their families.
- ECRI Institute initiated an annual list of top ten health technology hazards – and alarms have consistently been at the top of this list.
- National Association of Clinical Nurse Specialists (NACNS) constructed a six-sigma process including an Alarm Fatigue Toolkit recommending finding ways to define, measure and analyze alarm challenges to design methods for improvement.
- Healthcare Technology Foundation has created safety assessment tools to help in improving alarm safety by focusing on incorporating human, organizational and technical factors in an integrated approach.
If you can’t measure it, you can’t improve it
To understand the root causes and bottlenecks and drive improvements, and more importantly, provide continuous measurements and monitoring to sustain those improvements, one must be able to establish a baseline of various metrics related to root causes of clinical alarms.
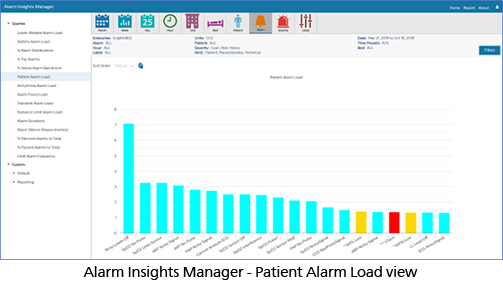
Philips Capsule Alarm Insights Manager (AIM) is a cloud-based solution that provides an interactive, intuitive set of alarm key performance indicators (KPIs) to assess alarm burden over hours, days, weeks, or months, by clinical unit, patient, alarm type or severity. These KPIs provide insights into root causes of alarms, thus arming our clinical consultants with evidence to establish recommendations and training with the goal of reducing non-actionable, nuisance and clinically irrelevant alarms.
Alarm Insights Manager also helps identify potentially actionable insights into hospital alarm system quality, with the aim of combating alarm fatigue and establishing best practices. It also allows benchmarking historically and across units for continuous improvement monitoring.
Philips Capsule’s Alarm Insights Manager supports healthcare’s quadruple aim in several ways.
By enabling a quieter and safer environment for the patient that promotes better sleep and less anxiety, Alarm Insights Manager can potentially enhance a patient’s healing process. Fewer nuisance alarms can mean less sensory and cognitive overload for clinicians, and less time responding to clinically irrelevant alarms, which can potentially allow for more focus on actionable events, with the goal of helping to improve patient care, potentially reducing errors and possibly leading to better experiences and outcomes for patients and staff.
Find out more about Philips Capsule Alarm Insights Manager and Clinical Insights Manager.
About the authors
Jennifer Rist is a Senior Product Manager for Clinical Analytics at Philips Capsule.
Youssef Abou-Hawili is a Fellow Architect Leader for Hospital Patient Monitoring Research & Development at Philips.
Learn more about Alarm Insights Manager and Clinical Insights Manager.
Download